Introduction
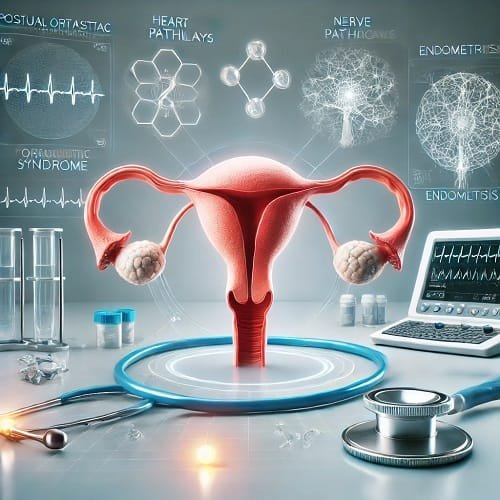
POTS and Endometriosis are two conditions that individually affect many people, particularly women, but their connection has only recently started to gain more attention. POTS syndrome, or Postural Orthostatic Tachycardia Syndrome, is a disorder of the autonomic nervous system that causes a rapid heart rate, dizziness, fatigue, and a variety of other symptoms when standing. Endometriosis, on the other hand, is a chronic condition where tissue similar to the lining of the uterus grows outside of it, often causing pelvic pain, heavy menstrual bleeding, and infertility.
While these two conditions might seem unrelated at first glance, there is growing recognition of the overlap between POTS and Endometriosis. Both conditions have a high incidence among women and share some common symptoms, including fatigue, chronic illness, and a dysfunctional autonomic nervous system. This overlap makes understanding the relationship between POTS and Endometriosis crucial for diagnosis and effective treatment.
The symptoms of POTS—like heart rate changes, dizziness, and lightheadedness—can be exacerbated by the hormonal fluctuations caused by Endometriosis. As a result, individuals suffering from both conditions may experience an especially challenging path to diagnosis and relief. Understanding how POTS and Endometriosis intersect can lead to more accurate diagnoses, better treatments, and a higher quality of life for those affected. Awareness and education are key to managing these complex conditions and improving care for the millions of women struggling with both.
Table of Contents
What is POTS and How Does It Relate to Endometriosis?
POTS and Endometriosis are two distinct yet often overlapping conditions that significantly impact a person’s quality of life. POTS syndrome, short for Postural Orthostatic Tachycardia Syndrome, is a disorder of the autonomic nervous system. It affects the body’s ability to regulate blood circulation and heart rate when changing positions, like standing up. This can lead to symptoms such as dizziness, fatigue, heart palpitations, and even fainting. Essentially, when someone with POTS stands, their blood pressure drops, and their heart compensates by increasing its rate, but the body doesn’t adjust properly. This disruption in the autonomic nervous system can cause chronic pain and fatigue, which are also common issues in Endometriosis.
Endometriosis, on the other hand, is a condition where tissue similar to the lining of the uterus grows outside it, often on other organs like the ovaries, fallopian tubes, or bowel. This tissue continues to act as it would in the uterus, shedding and causing severe pelvic pain, heavy menstrual bleeding, and in many cases, infertility. The endocrine disorders associated with Endometriosis contribute to hormonal fluctuations that can exacerbate other symptoms, including fatigue and generalized pain.
The overlap between POTS and Endometriosis occurs because both conditions impact the body’s regulation systems. For example, the autonomic dysfunction in POTS can worsen the chronic pain associated with Endometriosis, while the fatigue from Endometriosis can amplify the debilitating tiredness caused by POTS. Additionally, symptoms like dizziness and heart rate changes can be exacerbated in those who suffer from both, creating a vicious cycle that can be difficult to manage without proper care and diagnosis. Understanding how POTS and Endometriosis relate is essential for managing both conditions effectively.
7 Key Facts You Need to Know About POTS and Endometriosis
Understanding the relationship between POTS and Endometriosis is crucial for those affected by both conditions. Below are seven essential facts that shed light on how these two disorders intersect and the unique challenges they present.
1. POTS and Endometriosis Are Both Chronic Illnesses
Both POTS and Endometriosis are chronic illnesses that significantly impact daily life. POTS causes long-term issues with heart rate regulation and blood circulation, while Endometriosis leads to persistent pelvic pain, menstrual cycle disruptions, and hormonal imbalances. The ongoing nature of both conditions means that people affected by them must adopt long-term management strategies, often involving multiple specialists.
2. Hormonal Imbalance Exacerbates Symptoms
The hormone imbalance caused by Endometriosis can make POTS symptoms worse. Estrogen, a hormone that fluctuates throughout the menstrual cycle, has been linked to worsening autonomic dysfunction in POTS patients. This imbalance can increase heart rate issues, making it harder for individuals with both conditions to manage the physical symptoms. Recognizing how hormone imbalance influences both conditions is vital for effective treatment.
3. Autonomic Dysfunction Is a Common Factor
Both POTS and Endometriosis involve autonomic dysfunction, meaning that the body’s automatic systems, like blood flow regulation, are impaired. In POTS, the autonomic nervous system fails to regulate blood pressure and heart rate issues, causing dizziness and fainting. In Endometriosis, autonomic dysfunction can contribute to digestive issues, such as nausea, bloating, and GI issues, especially when combined with hormonal changes.
4. GI Issues Can Be More Severe
People with POTS and Endometriosis often experience GI issues such as nausea, bloating, and abdominal pain. The autonomic dysfunction in POTS can interfere with digestion, leading to slower gut motility, while Endometriosis can affect the bowel and other gastrointestinal organs. This double-whammy can create a challenging symptom management routine, as the two conditions interact in unpredictable ways.
5. Fatigue Is a Shared Symptom
Chronic fatigue is one of the most debilitating symptoms of both POTS and Endometriosis. The constant strain on the body’s systems from autonomic dysfunction, combined with the pain and inflammation from Endometriosis, creates an overwhelming sense of exhaustion. Those with both conditions may find that fatigue is not just a result of physical activity but also a constant underlying issue.
6. Pelvic Pain Can Worsen Heart Rate Issues
The chronic pain caused by Endometriosis can also trigger heart rate issues in POTS patients. When pain levels increase, it can activate the body’s stress response, which can lead to a spike in heart rate. This makes it more difficult to manage both conditions simultaneously. POTS and Endometriosis patients often report that their heart rate increases during episodes of pelvic pain, creating a cycle of worsening symptoms.
7. Treatment Requires a Multi-Disciplinary Approach
Managing POTS and Endometriosis effectively requires a multi-disciplinary approach that addresses both the autonomic dysfunction of POTS and the chronic pain and hormonal imbalance of Endometriosis. Many patients benefit from working with a team of specialists, including cardiologists, gynecologists, and pain management professionals. Tailored treatment plans, which may include lifestyle changes, medications, and therapy, are crucial for improving quality of life.
ALSO READ
Abortion and Endometriosis: What Every Woman Should Know
Is Endometriosis a Disability? Understanding the Impact
Common Symptoms of POTS and Endometriosis: Overlapping Indicators

One of the most challenging aspects of living with POTS and Endometriosis is the overlapping symptoms that make it difficult to distinguish between the two conditions. Both conditions affect multiple systems in the body, resulting in a range of chronic symptoms that often overlap. This section focuses on the shared symptoms between POTS and Endometriosis, helping patients and caregivers better understand how these conditions interact.
1. Dizziness and Lightheadedness
Both POTS and Endometriosis can cause dizziness and lightheadedness. In POTS, the autonomic dysfunction disrupts blood flow and regulation of the heart rate, leading to a drop in blood pressure when standing, which causes a sense of dizziness. On the other hand, Endometriosis can trigger dizziness during pain episodes, particularly if there is intense pelvic pain or nausea. The stress caused by the pain can cause a cascade of symptoms that impact the autonomic nervous system, contributing to lightheadedness.
2. Fatigue
Extreme fatigue is a hallmark symptom of both POTS and Endometriosis. For POTS patients, the body’s inability to regulate blood circulation leads to chronic tiredness, often accompanied by an overwhelming sense of exhaustion. In Endometriosis, fatigue is primarily driven by chronic pain and hormonal imbalances. The persistent pelvic pain, alongside nausea and other discomforts, can drain energy, leaving individuals feeling constantly tired. For those with both conditions, this fatigue can feel particularly debilitating and often leaves them unable to perform basic daily tasks.
3. Abdominal Pain and Bloating
Abdominal pain, bloating, and nausea are common in both conditions. POTS can cause GI issues such as nausea and bloating due to the autonomic dysfunction, which slows digestion. On top of this, Endometriosis often affects the bowels, leading to painful symptoms such as abdominal pain, bloating, and sometimes nausea. The inflammation caused by Endometriosis can disrupt gastrointestinal function, and when combined with the blood flow abnormalities from POTS, it exacerbates GI symptoms.
4. Tachycardia and Heart Rate Issues
Tachycardia—an abnormal increase in heart rate—is a defining symptom of POTS, but it can also be triggered by Endometriosis. When Endometriosis patients experience pain or stress, the body’s response can elevate heart rate and cause episodes of tachycardia. This overlap between the two conditions makes managing heart rate issues particularly challenging. While POTS causes tachycardia as a direct result of autonomic dysfunction, Endometriosis can indirectly exacerbate these symptoms through pain or pelvic discomfort.
5. Postural Symptoms
Postural symptoms like dizziness or fainting are common in POTS due to blood circulation issues when standing or changing positions. These symptoms are less common in Endometriosis, but severe pain or stress, especially from pelvic cramping or bloating, can mimic or exacerbate postural changes, leading to dizziness or fainting. For example, the postural symptoms in POTS—such as standing-induced dizziness—can become more pronounced in those with Endometriosis during a painful flare-up.
How POTS and Endometriosis Are Diagnosed

Diagnosing POTS and Endometriosis can be challenging due to their overlapping symptoms, which often leads to delayed or missed diagnoses. While POTS and Endometriosis are separate conditions, their symptoms frequently intersect, making it crucial to use a combination of diagnostic tests to distinguish between the two.
Diagnosing POTS
The diagnosis of POTS is typically confirmed through a variety of diagnostic tests that assess the autonomic nervous system and cardiovascular health. The tilt table test is one of the primary diagnostic tools used to confirm POTS. During this test, the patient is strapped to a table that tilts them from a horizontal to a vertical position, monitoring their heart rate and blood pressure changes. If there’s a significant increase in heart rate (typically 30 beats per minute or more) upon standing, without a corresponding drop in blood pressure, POTS is often suspected.
Additionally, EKGs and blood pressure tests are often conducted to assess the functioning of the cardiovascular system, ruling out other conditions that may mimic the symptoms of POTS.
Diagnosing Endometriosis
On the other hand, diagnosing Endometriosis generally begins with a pelvic exam to check for tenderness or abnormalities in the reproductive organs. However, the most definitive method is through medical imaging such as ultrasound or MRI, which can identify endometrial lesions or cysts in the pelvic region. A laparoscopy, a minor surgical procedure, remains the gold standard for diagnosing Endometriosis, as it allows doctors to directly view the pelvic organs and confirm the presence of endometrial tissue outside the uterus.
Challenges in Diagnosis
The overlap between the symptoms of POTS and Endometriosis—such as chronic pain, fatigue, dizziness, and nausea—can make it difficult for healthcare providers to pinpoint the cause of a patient’s discomfort. Often, patients are misdiagnosed or treated for one condition while the other remains unaddressed. Because POTS and Endometriosis share similar symptoms like fatigue and GI issues, it’s essential for healthcare providers to take a comprehensive approach, utilizing a combination of diagnostic tests to rule out other potential causes.
Treatment Options for Managing POTS and Endometriosis

Managing POTS and Endometriosis often requires a multidisciplinary approach due to the complexity and overlap of symptoms. Both conditions can significantly affect a person’s daily life, but with the right treatments, it’s possible to alleviate symptoms and improve quality of life. This section will explore various treatment options available for managing both POTS and Endometriosis, focusing on methods that can address both conditions simultaneously or in tandem.
1. Lifestyle Changes for Managing Symptoms
Lifestyle adjustments are one of the most effective ways to manage POTS and Endometriosis. POTS patients can benefit from strategies such as increasing salt and fluid intake, which can help maintain blood circulation and reduce symptoms like dizziness and fatigue. Regular physical activity, particularly exercises that strengthen the lower body and improve circulation, can also help manage POTS. In contrast, Endometriosis patients may benefit from lifestyle changes like avoiding triggers that worsen pelvic pain or inflammation, such as high-stress levels or certain foods.
For both conditions, diet changes can play a crucial role. A balanced diet rich in anti-inflammatory foods can help manage Endometriosis by reducing pelvic pain, while a high-sodium, high-fluid intake can aid in managing POTS symptoms.
2. Medication Options
Medications for managing POTS and Endometriosis are often prescribed to help control symptoms. For POTS, medications such as beta-blockers can be used to help control heart rate issues, while fludrocortisone or midodrine may help improve blood circulation and prevent dizziness when standing. In addition, SSRI medications (selective serotonin reuptake inhibitors) can sometimes be prescribed to manage symptoms of autonomic dysfunction associated with POTS.
For Endometriosis, hormonal therapies are often prescribed to help reduce pelvic pain and menstrual cycle disruptions. Birth control pills, IUDs, or hormone therapy can regulate hormones and reduce endometrial lesions. In some cases, gonadotropin-releasing hormone (GnRH) agonists are used to induce a temporary menopause-like state, thus alleviating pelvic pain associated with Endometriosis.
3. Physical Therapy and Exercise
Physical therapy plays a pivotal role in managing both POTS and Endometriosis. For POTS patients, physical therapy focuses on strengthening the body, particularly the core and legs, to improve blood circulation and reduce dizziness or lightheadedness when standing. For Endometriosis patients, pelvic physical therapy can help with pelvic pain and muscle tension related to Endometriosis, improving overall function and comfort.
4. Surgical Options
In more severe cases of POTS and Endometriosis, surgery may be necessary. For POTS patients, implantable devices like a pacemaker can sometimes be recommended to manage heart rate issues. However, this is only considered in extreme cases where other treatments have not been successful.
For Endometriosis, surgery can be an option for those with severe symptoms. Laparoscopic surgery is typically used to remove endometrial lesions and adhesions, thereby reducing pelvic pain and preventing further complications. In some cases, hysterectomy may be suggested if other treatments do not provide relief.
5. Combining Treatments for Optimal Results
The key to managing both POTS and Endometriosis effectively lies in a combination of treatments tailored to the individual’s needs. For example, a patient may benefit from using a combination of hormonal therapy to manage Endometriosis, along with beta blockers or fluid therapy to manage POTS symptoms. Additionally, integrating physical therapy for POTS with diet changes for Endometriosis can help manage both conditions concurrently.
Managing the Emotional and Mental Health Impact of POTS and Endometriosis

The emotional and psychological toll of dealing with chronic illnesses like POTS and Endometriosis is often underestimated. Both conditions, with their debilitating chronic pain, fatigue, and other symptoms, can severely affect mental health. Patients with POTS and Endometriosis may experience anxiety, depression, and other mental health challenges, making it essential to focus on emotional well-being.
The Psychological Toll of Chronic Illness
Chronic pain and the unpredictability of POTS and Endometriosis can lead to feelings of frustration and hopelessness. The stress of managing long-term symptoms can also contribute to depression and anxiety. Moreover, the inability to maintain a normal routine or participate in everyday activities can lead to social isolation, further exacerbating mental health struggles.
Coping Strategies and Support
Managing the emotional challenges associated with POTS and Endometriosis requires a combination of coping strategies. Therapy—whether cognitive behavioral therapy (CBT) or supportive counseling—can help individuals process the emotional toll of chronic illness. Mindfulness practices, such as meditation or deep breathing exercises, can help manage stress and alleviate feelings of anxiety.
Joining support groups for those with POTS and Endometriosis can be incredibly beneficial, as it offers patients a community where they can share experiences and provide mutual support. These groups can help reduce feelings of isolation and offer coping strategies that may not be readily available from healthcare providers.
Conclusion: Building Awareness and Support for POTS and Endometriosis
In conclusion, POTS and Endometriosis are two complex and often misunderstood conditions that significantly affect the lives of those who suffer from them. Despite their overlap in symptoms, both conditions require a unique and tailored approach to diagnosis and treatment. Building awareness and support for POTS and Endometriosis is essential in helping patients find the resources, treatments, and communities they need to manage their symptoms.
Advocacy and Patient Education
Raising awareness about these conditions is crucial in improving diagnosis rates and ensuring that more people receive the care they need. Advocating for POTS and Endometriosis helps create more opportunities for research, treatment development, and support systems for those affected by these conditions.
Patients and caregivers should seek education and support to better understand how to manage POTS and Endometriosis and improve their quality of life. With the right resources and understanding, those affected by POTS and Endometriosis can lead fulfilling lives despite the challenges they face.
FAQ Section:
Can POTS and Endometriosis be treated together?
Yes, POTS and Endometriosis can be managed together through a combination of treatments, including medication, lifestyle changes, and physical therapy.
What are the most common symptoms of POTS and Endometriosis?
POTS symptoms include dizziness, fatigue, and tachycardia, while Endometriosis symptoms include pelvic pain, bloating, and menstrual irregularities.
How does POTS affect menstrual cycles?
POTS can exacerbate menstrual cycle irregularities, especially since both conditions impact the autonomic nervous system and can influence hormone levels.
Is POTS a life-threatening condition?
POTS is generally not life-threatening but can significantly affect quality of life. Treatment focuses on managing symptoms and improving overall function.