Jump to Section
Introduction
Menopause is a significant phase in a woman’s life, marked by numerous physical changes, including the onset of frozen shoulder during menopause. While many women associate menopause with symptoms like hot flashes and mood swings, one lesser-known issue is shoulder pain during menopause. The connection between frozen shoulder treatment and menopause has gained attention in recent years, as more women experience the discomfort of shoulder stiffness and pain during this period of hormonal changes.
As estrogen levels drop during menopause, many women report experiencing menopause and joint pain, particularly in the shoulders. The result is often menopause shoulder stiffness and restricted arm movement, making even simple daily tasks more difficult. This condition, commonly referred to as frozen shoulder, can leave women feeling frustrated and debilitated.
In this article, we’ll explore the causes behind frozen shoulder in the menopause phase of the women, the symptoms that accompany it, and effective solutions to ease the discomfort. We’ll also dive into natural remedies and lifestyle changes that can provide relief and help prevent future episodes. If you’re struggling with frozen shoulder pain during menopause, this guide will provide you with practical and effective ways to regain mobility and comfort. Let’s begin by understanding what does it mean by frozen shoulder for women in their menopause phase and how it affects women during this phase of life.
Understanding Frozen Shoulder and Menopause
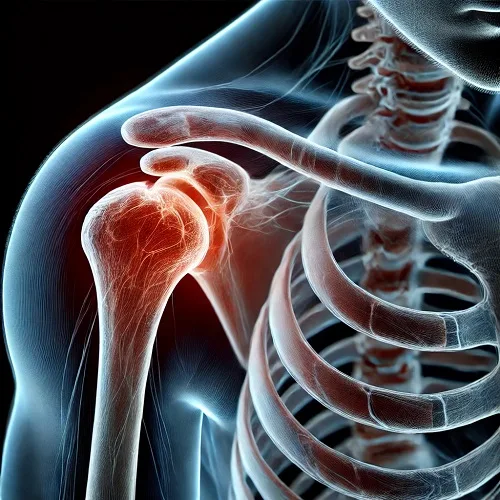
Frozen shoulder during menopause is a condition that many women experience during the transitional period of menopause. This painful and debilitating disorder occurs when the shoulder becomes stiff and painful, leading to limited mobility. It’s closely linked to the hormonal fluctuations that occur during menopause, which affect the body’s joints and tissues. Women going through menopausal symptoms may notice an increase in shoulder pain or stiffness, which can eventually lead to frozen shoulder, also known as adhesive capsulitis.
During menopause, the body undergoes a series of hormonal changes, primarily a decrease in estrogen levels. Estrogen plays a significant role in maintaining joint health, including keeping the tissues and ligaments flexible. As estrogen levels drop, women may experience joint inflammation, which contributes to stiffness and discomfort in the shoulder joint. This is one of the primary reasons behind the onset of this condition.
The process of developing frozen shoulder typically happens in three stages: freezing, frozen, and thawing. The freezing stage is where the pain begins, followed by the frozen stage, where the shoulder becomes increasingly stiff. Lastly, the thawing stage involves a gradual return of motion, though this can take months or even years. The connection between frozen shoulder and menopause and hormonal fluctuations is particularly significant in the freezing and frozen stages, where inflammation and tissue thickening are most pronounced.
Common symptoms include shoulder stiffness, sharp pain that worsens with movement, and a noticeable limitation in the range of motion. Women may find it difficult to perform everyday activities like dressing, lifting objects, or even reaching behind their back. Diagnosis is typically based on physical exams and imaging tests to rule out other conditions.
Understanding the link between frozen shoulder and hormonal changes is key to managing the pain and discomfort. By addressing the root causes, women can find effective ways to relieve the symptoms and regain shoulder mobility.
Symptoms of Frozen Shoulder During Menopause

Frozen shoulder during menopause can be incredibly painful and disruptive. Women going through menopause may experience a range of symptoms that gradually worsen, often starting with pain in the shoulder and progressing to more severe restrictions in movement. Understanding these symptoms is crucial for managing the condition effectively.
The stiffness associated with frozen shoulder is the hallmark of this condition. In the early stages, women may notice a dull, aching pain that worsens with movement. This pain often starts in the shoulder joint and radiates down the arm, affecting daily activities like reaching overhead or lifting objects. As the condition progresses, restricted arm movement becomes more pronounced, making it difficult to perform even simple tasks like dressing or carrying groceries.
Frozen shoulder develops in three distinct stages: freezing, frozen, and thawing. During the freezing stage, the shoulder becomes increasingly painful and stiff, leading to a gradual loss of range of motion. The frozen stage is characterized by significant stiffness, with less pain but a further reduction in movement. Finally, in the thawing stage, the pain and stiffness begin to subside, but regaining full mobility can take months or even years. For women experiencing frozen shoulder during menopause, hormonal changes often intensify these stages, making it harder to recover quickly.
It’s important to consult a doctor if the pain becomes severe or if there’s a significant loss of mobility. Shoulder pain relief strategies, including physical therapy and medical treatments, can help alleviate discomfort and promote healing. If left untreated, the condition can lead to chronic pain and long-term functional limitations.
Causes of Frozen Shoulder During Menopause

The connection between frozen shoulder and hormonal changes is key to understanding why women experience this condition. As women transition through menopause, their body undergoes significant hormonal imbalance, with a sharp decline in estrogen levels. Estrogen plays a crucial role in maintaining joint flexibility and cushioning the connective tissues. When estrogen levels drop, it can lead to increased stiffness, pain, and even swelling in the joints, contributing to frozen shoulder.
One of the most noticeable effects of estrogen decline is on collagen production. Collagen is a vital protein that provides structure and strength to the tendons, ligaments, and tissues around the shoulder. As estrogen levels fall during menopause, collagen production decreases, leading to weaker and less flexible tissues. This loss of elasticity and the tightening of the shoulder capsule are key contributors to this frozen shoulder. Without adequate collagen, the shoulder joint becomes more susceptible to joint pain and stiffness.
Another factor at play is inflammation. The hormonal changes that occur during menopause can increase inflammation in the body, particularly in the joints. This inflammation can aggravate the condition of frozen shoulder, making the symptoms more intense and harder to manage. In addition, the tissue around the shoulder joint may thicken and become less mobile, further restricting movement and causing pain.
As a result, frozen shoulder in menopause is a direct consequence of the hormonal shifts that occur during this phase of life. Women dealing with this condition often find that the decline in estrogen levels, combined with changes in collagen production and increased inflammation, leads to painful and debilitating stiffness in the shoulder joint.
Effective Treatment Options for Frozen Shoulder During Menopause
When dealing with this shoulder problem, managing the condition effectively is essential to reducing pain and improving mobility. There are several frozen shoulder treatment options available, ranging from medical interventions to natural remedies. Let’s explore these treatment options in detail, so you can find the best solutions for relieving your symptoms.
Medical Treatments
One of the most common treatments for frozen shoulder is physical therapy. A physical therapist can guide you through specific frozen shoulder exercises designed to improve range of motion, increase flexibility, and reduce stiffness. These exercises help break up scar tissue that forms in the shoulder joint and gradually restore movement. Physical therapy is often the first line of defense when treating frozen shoulder, as it targets the root of the problem—restricted movement.
In some cases, medications for frozen shoulders may be prescribed to help manage pain and inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen are often recommended to reduce swelling and relieve discomfort. For more severe cases, doctors may suggest corticosteroid injections to reduce inflammation in the shoulder joint. These injections can provide temporary relief, allowing you to engage more easily in joint exercises and physical therapy.
Exercise and Stretching
Regular frozen shoulder exercises and stretching routines are essential in promoting healing and regaining movement in the shoulder joint. Specific stretches can help to gently increase flexibility and ease the tension that contributes to frozen shoulders. Key exercises often include shoulder rolls, pendulum swings, and wall climbs to help improve motion. A physical therapist can tailor these exercises to your specific needs, ensuring that they are effective and safe.
Staying active and consistent with these joint exercises is crucial for long-term recovery. They can prevent the shoulder from becoming stiffer over time and improve overall shoulder function.
Home Remedies and Natural Approaches
In addition to medical treatments and exercises, hot and cold therapy can be incredibly helpful for alleviating the pain associated with frozen shoulders during this phase of life. Applying a warm compress or heating pad can increase blood flow to the shoulder and relax tight muscles, while a cold pack can help reduce swelling and numb the pain. Alternating between hot and cold therapy throughout the day can offer significant relief and improve comfort.
Additionally, following an anti-inflammatory diet can help reduce the internal inflammation that contributes to frozen shoulder. Foods rich in omega-3 fatty acids, such as salmon and flaxseed, as well as antioxidants from fruits and vegetables, can aid in reducing inflammation. Staying hydrated and avoiding processed foods high in sugars can also support overall joint health.
By combining medical treatments, regular frozen shoulder exercises, and natural remedies like hot and cold therapy, you can effectively manage the symptoms of frozen shoulder and regain mobility in your shoulder.
RELATED POSTS
Itchy Ears in Menopause? What No One Tells You
Stop Menopause Bloating: 5 Proven Solutions That Work
Centrum Menopause: Best Multivitamins for Smooth Transition
Stop Vaginal Odor During Menopause – Here’s How!
Transform Your Health: 7-Day Menopause Diet Plan for Results
Natural Remedies and Lifestyle Changes for Frozen Shoulder Relief

When managing frozen shoulders, many women turn to natural remedies to complement traditional treatments. These alternative approaches can provide significant relief from pain and stiffness, supporting long-term recovery and improving overall quality of life. Let’s explore some of the most effective natural remedies for frozen shoulder and lifestyle changes that can help ease the discomfort associated with this condition.
Herbal Treatments and Alternative Therapies
Herbal treatments have been used for centuries to alleviate joint pain and inflammation, and they can be incredibly effective for this problem. Herbs such as turmeric, ginger, and boswellia are known for their anti-inflammatory properties. Turmeric, in particular, contains curcumin, a powerful compound that helps reduce swelling and pain in the joints. You can incorporate these herbs into your diet or use them in the form of supplements to support joint health.
Acupuncture and massage therapy are also popular alternative treatments. Acupuncture can help relieve pain by stimulating specific pressure points along the body, promoting blood flow and reducing inflammation. Similarly, regular massage therapy can target the shoulder area, helping to relieve muscle tension and increase circulation. These therapies not only reduce pain but also promote relaxation and improved mobility.
Lifestyle Changes for Pain Relief
Incorporating certain lifestyle changes can significantly ease the pain associated with frozen shoulders during menopause. Stress reduction techniques such as deep breathing exercises, meditation, or mindfulness can help reduce the tension that contributes to shoulder pain. Stress often exacerbates inflammation in the body, so managing emotional and physical stress is key to healing.
Additionally, a diet rich in anti-inflammatory foods plays a crucial role in joint health. Eating foods high in omega-3 fatty acids, such as fatty fish like salmon, chia seeds, and walnuts, can reduce inflammation and promote healing in the shoulder. Fresh fruits and vegetables, especially leafy greens and berries, are packed with antioxidants that help combat inflammation. Limiting processed foods and sugary snacks is also important for reducing overall body inflammation.
Exercises for Joint Flexibility and Relaxation
Incorporating regular exercise is essential for improving flexibility and reducing stiffness in the shoulder. Practices like yoga for menopause and tai chi focus on gentle movements and stretches that promote joint flexibility and relaxation. These exercises are particularly beneficial for women with frozen shoulder in this phase of women’s life, as they help to alleviate tension and increase mobility without causing additional strain on the body. Yoga and tai chi also incorporate deep breathing techniques, which can enhance stress reduction and improve overall well-being.
By combining natural remedies with healthy lifestyle changes, you can significantly improve your recovery and manage the discomfort associated with this problem.
Prevention Tips to Avoid Frozen Shoulder During Menopause

Preventing from frozen shoulder during the menopause era involves taking proactive steps to maintain joint health and flexibility, especially as hormonal changes during menopause can increase the risk of joint pain and stiffness. By following a few simple guidelines, women can significantly reduce their chances of developing frozen shoulder and promote overall well-being.
Maintaining Good Posture
One of the most effective ways to prevent frozen shoulder is by practicing proper posture correction. Poor posture can put added strain on the shoulder joints, leading to stiffness and discomfort. When sitting or standing, make sure to align your shoulders, keeping them relaxed and pulled back. This reduces unnecessary tension in the shoulder area and helps prevent the buildup of stiffness that can lead to frozen shoulder.
Stay Active and Perform Regular Stretching Exercises
Staying active is crucial for preventing joint pain and promoting healthy shoulders. Menopause exercises that focus on shoulder mobility, such as gentle stretches and strength training, can help keep the shoulder joints flexible and strong. Simple exercises like shoulder rolls, arm circles, and gentle neck stretches can encourage movement and keep the muscles around the shoulder flexible. Regular movement helps to prevent the shoulder from becoming rigid and promotes blood flow to the area.
Hydrate and Nourish Your Joints
Keeping your joints well-hydrated and nourished is essential for maintaining their health and preventing stiffness. Drinking plenty of water helps lubricate the joints, reducing the risk of friction and inflammation. Additionally, a nutrient-rich diet that includes omega-3 fatty acids, antioxidants, and vitamins like vitamin D and calcium supports joint health and reduces the likelihood of developing this problem. Focus on foods like leafy greens, fatty fish, and nuts to keep your joints in top condition.
Weight Management and Healthy Habits
Maintaining a healthy weight is another key factor in reducing the risk of this condition. Excess weight puts additional stress on the joints, leading to inflammation and increasing the likelihood of joint pain. By following a balanced diet, staying active, and practicing portion control, you can reduce the burden on your joints and promote overall health. Healthy habits like regular exercise, adequate sleep, and stress management also contribute to joint health and can prevent frozen shoulder from developing.
By following these prevention tips, you can significantly reduce the risk of this condition and enjoy better mobility, comfort, and overall well-being.
When to Seek Medical Help for Frozen Shoulder
While many cases of frozen shoulder can be managed with home remedies and lifestyle changes, there are times when seeking professional medical help is necessary. If you experience severe shoulder pain that doesn’t improve with rest or over-the-counter treatments, it’s important to consult a doctor for frozen shoulder. Persistent pain, especially if it interferes with daily activities, could be a sign that the condition requires medical intervention.
Another indication that you should seek a medical evaluation is when you notice a significant limited range of motion in your shoulder. If basic movements, like raising your arm or reaching behind your back, become nearly impossible, it’s time to see a doctor. A healthcare provider can perform a physical examination and may recommend imaging tests, such as an X-ray or MRI, to confirm the diagnosis and rule out other conditions.
Consulting a doctor early can lead to a more tailored treatment plan, potentially involving physical therapy, medications, or injections to reduce inflammation and improve mobility. By addressing this condition early, you can avoid long-term complications and regain full use of your shoulder more quickly.
Frequently Asked Questions (FAQs)
Can menopause cause frozen shoulder?
Yes, menopause is often linked to the hormonal changes women experience. A decline in estrogen levels can lead to joint stiffness and inflammation, particularly in the shoulder resulting frozen shoulders.
How long does frozen shoulder last during menopause?
The duration of frozen shoulder varies. It can take anywhere from several months to up to 3 years for the shoulder to fully recover, depending on the severity of the condition and the treatments used.
What is the best treatment for frozen shoulder during menopause?
The best treatment for frozen shoulder often involves a combination of physical therapy, frozen shoulder exercises, and pain relief for frozen shoulder. In more severe cases, corticosteroid injections or surgery may be recommended.
Can frozen shoulder be prevented during menopause?
Yes, by maintaining good posture, staying active, and performing regular menopause exercises, you can reduce the risk of frozen shoulder. Keeping your joints hydrated and nourished is also key.
How can I relieve shoulder pain during menopause?
Shoulder pain during menopause can be relieved through natural remedies like hot and cold therapy, anti-inflammatory diets, and regular stretches. Physical therapy and medication are also effective options.
What are the common symptoms of frozen shoulder during menopause?
Symptoms of frozen shoulder in menopause include shoulder stiffness, pain that worsens with movement, and limited range of motion in the affected shoulder.
Is physical therapy effective for frozen shoulder during menopause?
Yes, physical therapy is one of the most effective ways to treat frozen shoulder. It helps increase flexibility, reduce stiffness, and improve mobility in the shoulder joint.
Can hormone therapy help with frozen shoulder during menopause?
While hormone therapy can help alleviate other menopause symptoms, it may not directly address frozen shoulder. However, it may reduce overall inflammation, which can have an indirect benefit.
What exercises can help with frozen shoulder during menopause?
Gentle frozen shoulder exercises such as shoulder rolls, pendulum swings, and wall climbs can improve flexibility and reduce pain. Consulting with a physical therapist is recommended to ensure the exercises are appropriate.
Does weight gain affect frozen shoulder during menopause?
Yes, excess weight can put additional stress on your joints, including the shoulder, increasing the risk of joint pain menopause and worsening frozen shoulders. Maintaining a healthy weight is important for preventing this condition.
Can I still do yoga for frozen shoulder during menopause?
Yes, yoga for menopause can be beneficial for improving flexibility and relieving pain. Focus on gentle poses that target the shoulders and promote relaxation.
How does stress affect frozen shoulder during menopause?
Stress can contribute to muscle tension and inflammation, which can worsen frozen shoulder in menopause. Stress reduction techniques like deep breathing, meditation, and yoga can help alleviate some of this tension.
Is surgery necessary for frozen shoulder during menopause?
Surgery is generally a last resort when other treatments like physical therapy, medications, and injections do not provide sufficient relief for frozen shoulder during menopause. Most cases improve with non-invasive treatments.
Are there any dietary changes that help with frozen shoulder during menopause?
Yes, incorporating anti-inflammatory foods such as omega-3 fatty acids from fatty fish, leafy greens, and berries can help reduce inflammation and support joint health.
What’s the role of estrogen in frozen shoulder during menopause?
Estrogen decline during menopause plays a major role in frozen shoulder during menopause. Lower estrogen levels can lead to reduced collagen production, which results in stiffer and less flexible tissues around the shoulder joint.
Conclusion
In conclusion, frozen shoulder during menopause can be a challenging condition, but with the right treatment and proactive steps, you can manage and alleviate the symptoms. From medical treatments like physical therapy and corticosteroid injections to natural remedies such as shoulder pain remedies and hot and cold therapy, there are several ways to reduce pain and restore mobility. Prevention strategies, including maintaining good posture, staying active, and incorporating menopause exercises, are also key in avoiding the onset of frozen shoulder.
It’s important to take charge of your health and implement these lifestyle changes to improve your shoulder health. If the pain persists or limits your mobility, don’t hesitate to seek professional medical advice. Early intervention is crucial for effective treatment of frozen shoulder and managing menopause pain.
References
Medical News Today: Frozen Shoulder and Menopause: Link and How to Treat
Puget Sound Orthopaedics: The Do’s and Don’ts for Frozen Shoulder
Midi: Frozen Shoulder During Menopause: Causes, Symptoms, and Treatment
Orthoinfo: Frozen Shoulder – Adhesive Capsulitis – OrthoInfo – AAOS
Simply Menopause: Link Between Frozen Shoulder and Menopause






